
Condition Descriptions
A convenient list of these conditions with links to these descriptions can be found on our “Conditions” page. Note: Work in progress
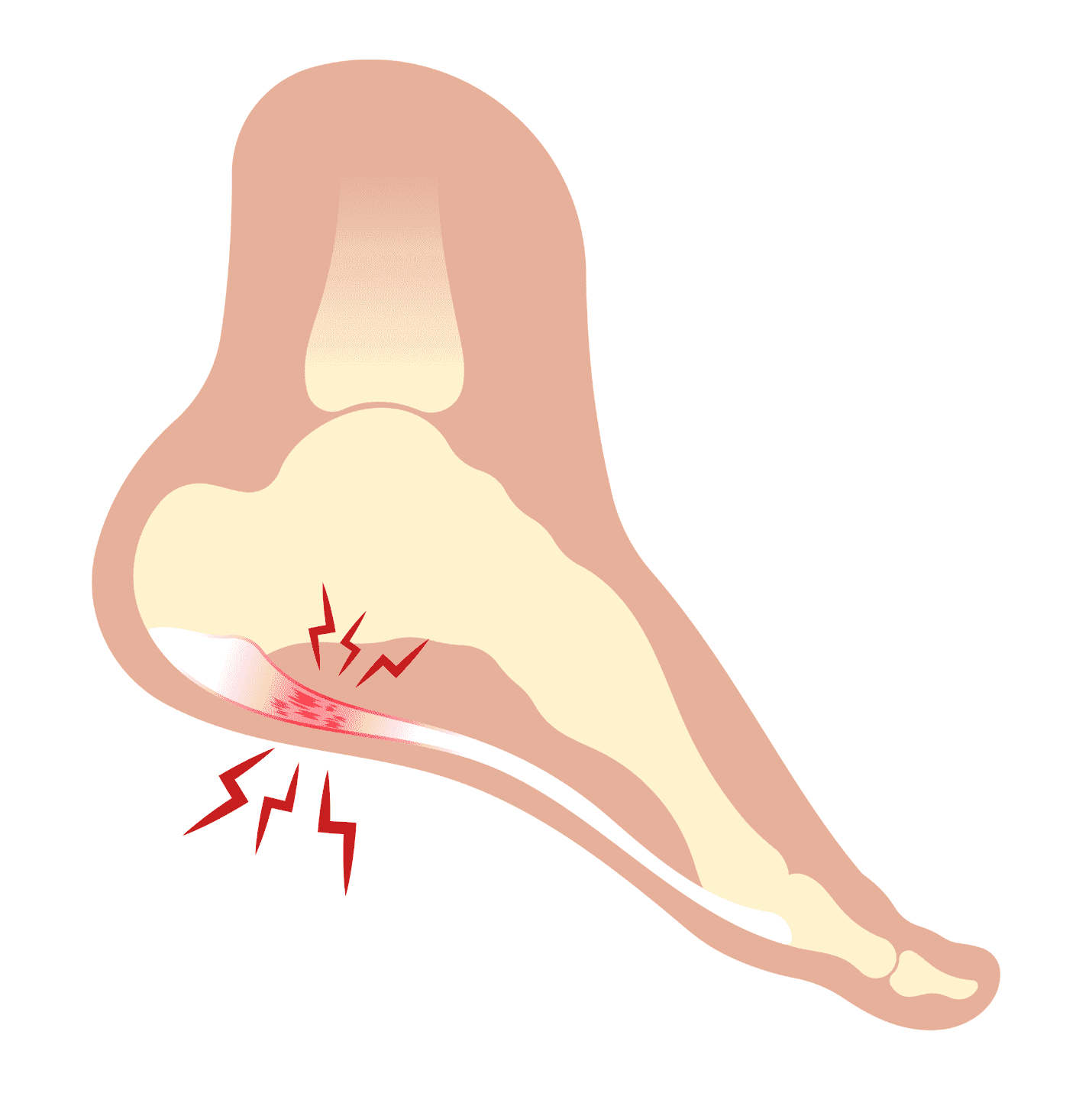
Plantar Fasciitis
What is Rotator Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. It happens when the plantar fascia—a thick band of tissue that runs along the bottom of your foot from your heel to your toes—becomes irritated or inflamed. This condition often develops gradually and is especially noticeable with the first steps in the morning or after long periods of sitting or standing.
Common symptoms include:
Sharp or stabbing pain in the heel
Pain that’s worse in the morning or after rest
Discomfort after standing or walking for long periods
Tightness in the arch or calf
Plantar fasciitis is often caused by repetitive stress and overuse. It’s more likely to develop in people who:
Stand or walk frequently on hard surfaces
Have flat feet or high arches
Wear unsupportive footwear
Have tight calf muscles or Achilles tendons
Are physically active or run regularly
Are overweight
Physical therapy is a highly effective, non-invasive treatment for plantar fasciitis. The goal is to reduce pain, promote healing, and prevent the condition from returning. Treatment may include:
Stretching and mobility exercises for the plantar fascia, Achilles tendon, and calf
Strengthening exercises to improve foot and ankle stability
Hands-on manual therapy to reduce stiffness and improve circulation
Gait and posture training to correct movement patterns
Taping or orthotic support to reduce strain during daily activities
Education on footwear choices and modifying daily routines
Other treatment options may include:
Rest and ice to calm inflammation
Supportive footwear or custom shoe inserts
Over-the-counter anti-inflammatory medications (with your doctor’s guidance)
Night splints to gently stretch the plantar fascia while sleeping
Corticosteroid injections in more severe or prolonged cases
Shockwave therapy or other advanced interventions if pain persists
Surgery is rarely necessary and typically only considered after conservative treatments have been tried without success.
Patellofemoral Pain Syndrome
Patellofemoral Pain Syndrome, often called “runner’s knee,” is a condition that causes pain around the front of the knee, especially behind or around the kneecap (patella). It often develops from overuse, muscle imbalances, or improper movement patterns that cause the kneecap to track incorrectly as you move.

People with PFPS may notice:
A dull, aching pain in the front of the knee
Pain during activities like running, squatting, climbing stairs, or sitting with the knees bent for long periods
A feeling of the knee “giving out” or feeling unstable
While it’s common in runners and active individuals, it can affect anyone — especially those who increase their activity level too quickly or have muscle weakness in the hips, thighs, or core.
How is it Treated?
There are several ways to treat patellofemoral pain syndrome, but physical therapy is one of the most effective, long-term solutions.
How Physical Therapy Helps:
Physical therapists are movement specialists who can help identify and correct the root causes of your knee pain. Your treatment plan may include:
Strengthening Exercises
Targeted exercises to strengthen the muscles around the knee, particularly the quadriceps, glutes, and hip muscles, which help stabilize the kneecap during movement.Stretching Tight Muscles
Tight muscles, such as the hamstrings, calves, or iliotibial (IT) band, can pull on the knee in ways that cause pain. Your therapist will guide you through stretches to improve flexibility and reduce strain.Movement Retraining
Your therapist may observe how you walk, run, or squat to identify poor movement patterns. With proper coaching and cues, they can help you move more efficiently and reduce stress on your knees.Taping or Bracing (if needed)
In some cases, taping techniques can temporarily improve kneecap alignment and reduce pain during activity.Education and Activity Modification
Your therapist will help you understand what activities may aggravate your symptoms and how to modify them. They’ll also guide you through a safe return to the activities you love.
Other Treatment Options
While physical therapy should be the first line of treatment, other options may include:
Rest and activity modification
Ice and anti-inflammatory medications
Shoe inserts (orthotics) if foot mechanics contribute to the problem
In rare cases, surgical intervention (usually only if other treatments fail)
The Bottom Line
Patellofemoral pain syndrome is a common and treatable condition. With the right care — especially a guided physical therapy program — most people can return to full activity without surgery. If you’re struggling with knee pain, physical therapy can help you move better, feel better, and get back to doing the things you enjoy.
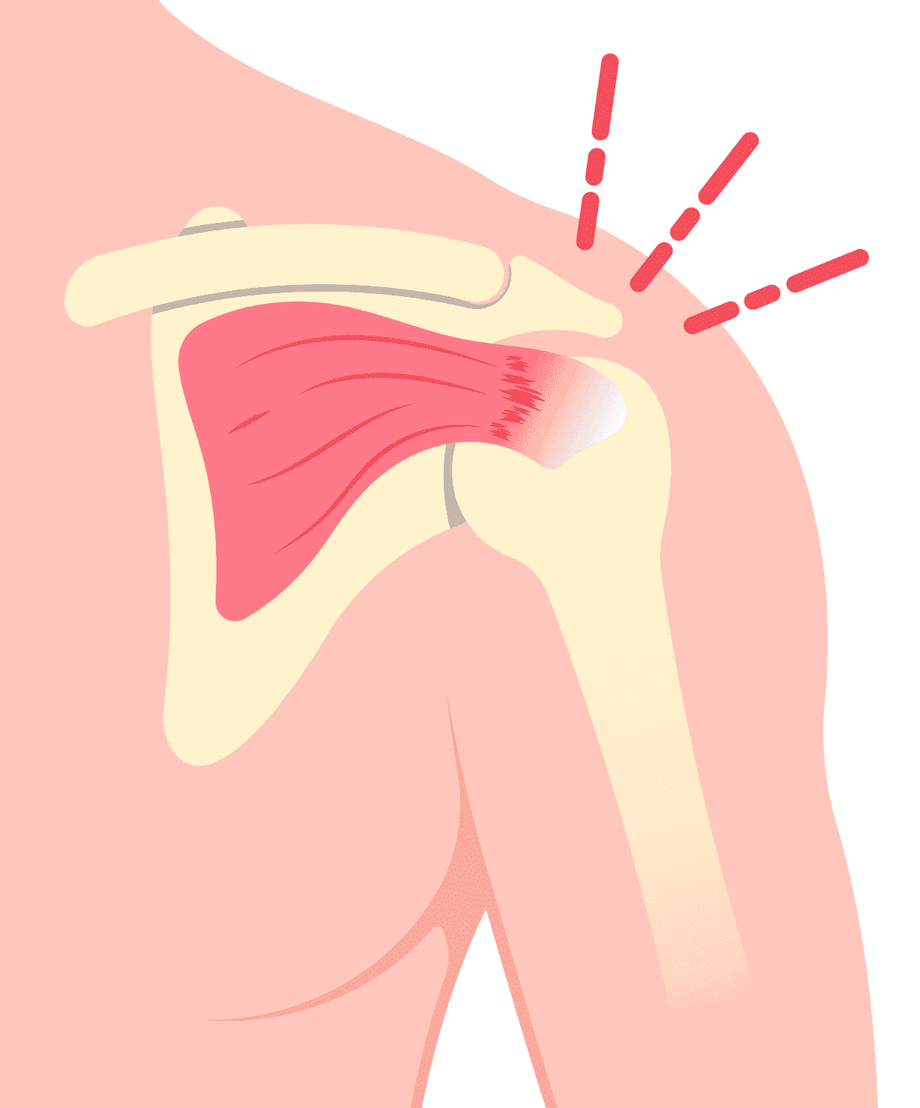
Rotator Cuff Issues
What is Rotator Cuff Pathology?
Rotator cuff pathology refers to problems affecting the group of muscles and tendons that help move and stabilize your shoulder. These muscles and tendons form the “rotator cuff,” which keeps the ball of your upper arm bone centered in the shoulder socket and allows you to lift, reach, and rotate your arm.
What Can Go Wrong?
Over time, or after an injury, the rotator cuff can become irritated, strained, or torn. These issues can develop from overuse (especially with repetitive overhead movements), poor posture, natural wear and tear with age, or trauma like a fall or lifting something too heavy.
Common Types of Problems Include:
Tendonitis: Inflammation of the tendons, often from overuse
Impingement: The tendons get pinched between bones during movement
Partial or Full-Thickness Tears: Small or complete tears in the tendons, either from injury or degeneration over time
Common Symptoms:
Pain in the shoulder, especially when lifting the arm or reaching overhead
Weakness in the arm
Trouble sleeping on the affected side
Limited range of motion or a “catching” feeling with movement
Why It Matters:
If left untreated, rotator cuff problems can get worse and make everyday tasks—like getting dressed, reaching for a shelf, or carrying groceries—painful and difficult.
How Physical Therapy Helps:
Physical therapy can reduce pain, restore strength, and improve mobility. Treatment often includes:
Gentle stretching and strengthening exercises
Manual techniques to reduce tightness and improve movement
Posture training
Education on how to avoid further strain
In more severe cases, other treatments like injections or surgery may be needed—but many people improve with physical therapy alone.
Temporomandibular Disorder (TMD)
What is Temporomandibular Joint Disorder (TMD)?
Temporomandibular Joint Disorder, or TMD, refers to problems with the jaw joint and the muscles around it. This joint connects your lower jaw to the side of your head, and it’s what allows you to open and close your mouth, chew, speak, and even yawn. When something goes wrong with how this joint or the surrounding muscles work, it can cause pain, discomfort, and difficulty with jaw movement.

Why Does It Happen?
The jaw joint is a complex structure that needs to move smoothly and evenly. If the joint becomes irritated, if the disc inside the joint shifts out of place, or if the muscles become tight or overworked, it can lead to TMD. Things like clenching your teeth, grinding at night, poor posture, or even stress can put extra strain on the jaw and cause symptoms to develop.
Who is Most Affected?
TMD is most common in:
Adults between the ages of 20 and 40
Women (they tend to be affected more often than men)
People who are under a lot of stress or who grind their teeth
Common Symptoms:
Pain or soreness in the jaw, face, or around the ear
Clicking, popping, or locking when opening or closing the mouth
Trouble opening the mouth wide
Headaches or neck aches
A tired feeling in the jaw after chewing
Feeling like your bite is “off” or doesn’t line up right
How Can Physical Therapy Help?
Physical therapists can play a big role in helping people manage and recover from TMD. Our goals are to reduce pain, improve jaw movement, and fix any posture or muscle issues that are contributing to the problem.
Treatment might include:
Hands-on techniques to relax tight jaw muscles or gently move the jaw to improve how it works
Stretches and exercises to strengthen and improve control of the jaw and neck
Posture training to reduce stress on the jaw, especially if you tend to slouch or hold your head forward
Tips for daily habits, like how to avoid clenching your teeth, better sleeping positions, and ways to reduce stress on your jaw
Relaxation techniques to help manage stress or jaw tension
Other Treatment Options (Often Combined with PT):
Mouth guards or splints, made by a dentist, to prevent grinding or take pressure off the jaw
Medications like pain relievers or muscle relaxers
Counseling or stress management for those whose symptoms are linked to anxiety or habits like clenching
Injections, such as Botox, for severe muscle tightness
Surgery, in rare cases where nothing else helps
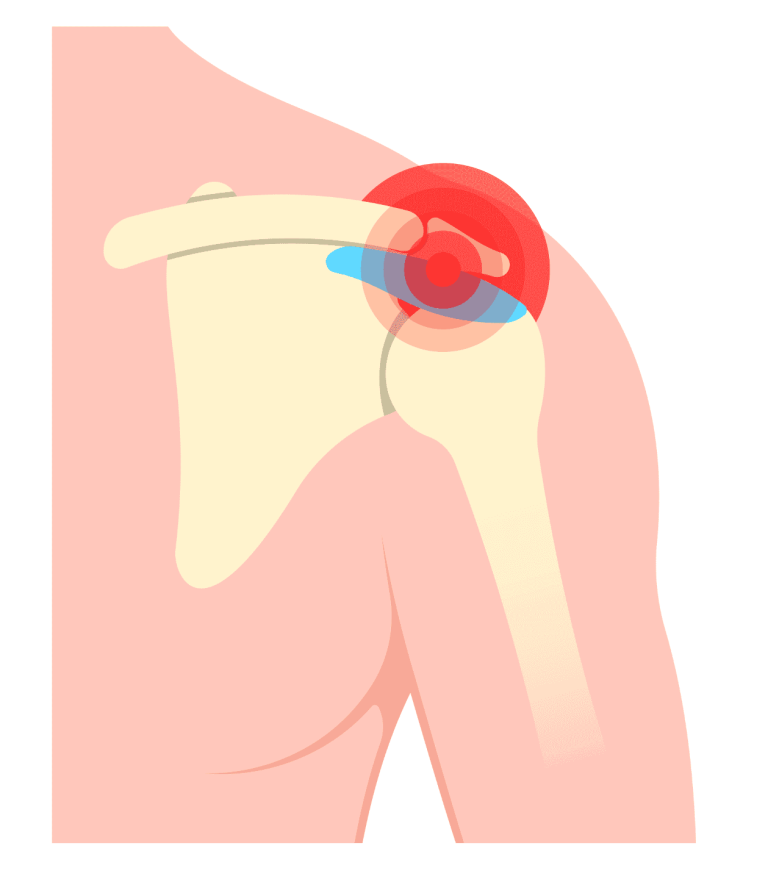
Shoulder Impingement
What is Shoulder Impingement?
Shoulder impingement is a common cause of shoulder pain, especially in people who perform repetitive overhead movements. It occurs when the tendons or bursa in the shoulder become pinched or irritated as they pass through a narrow space in the shoulder joint. This can lead to inflammation, pain, and limited range of motion.
Common symptoms include:
Pain when lifting the arm, especially overhead or out to the side
Pain or discomfort during reaching, throwing, or sleeping on the affected shoulder
Weakness in the shoulder or arm
A feeling of stiffness or catching during movement
Shoulder impingement often develops gradually due to overuse or poor movement mechanics. It is more likely to occur in people who:
Perform repetitive overhead activities (e.g., athletes, painters, mechanics)
Have poor posture or rounded shoulders
Have muscle imbalances or weakness in the shoulder or upper back
Experience shoulder instability or prior injuries
Are older adults with age-related changes in the shoulder joint
Physical therapy is a proven and effective treatment for shoulder impingement. The focus is on reducing pain, restoring movement, and preventing future irritation. Treatment may include:
Stretching exercises to improve flexibility in the shoulder and chest
Strengthening exercises for the rotator cuff and upper back muscles
Postural training to correct alignment and relieve pressure on shoulder structures
Manual therapy to reduce stiffness and improve joint mobility
Activity and movement modification to avoid aggravating positions
Education on ergonomics and body mechanics during work, sports, or daily tasks
Other treatment options may include:
Rest and ice to reduce inflammation
Over-the-counter anti-inflammatory medications (as recommended by your doctor)
Corticosteroid injections to decrease severe or persistent inflammation
Temporary activity modification to allow the shoulder to heal
Surgery in rare cases when conservative treatments do not provide relief
